Procedure
The following procedure takes a midline approach. Non-midline approaches are covered in the reference text Wildsmith, Armitage and McClure (2002).
Stage 1
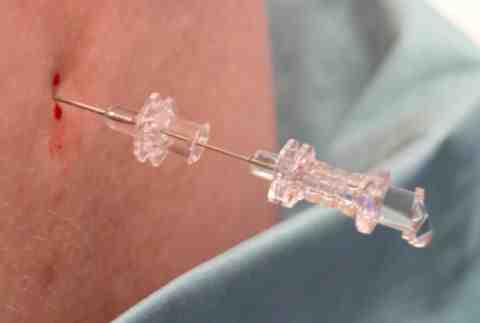
After the skin and subcutaneous tissues are infiltrated with local anaesthetic, the introducer is inserted in the midline at the mid-point of the chosen interspace, initially perpendicular to the back in all planes. If this is not possible, the direction can be adjusted at this stage.

The following procedure takes a midline approach. Non-midline approaches are covered in the reference text Wildsmith, Armitage and McClure (2002).
Stage 2
The spinal needle is inserted through the introducer and gently advanced. There is usually slight resistance to advancement. Strong resistance may be felt, especially in thick ligaments. Absolute resistance suggests bone has been encountered and re-direction is needed. Sometimes a slight loss of resistance or a faint pop may be felt as the needle tip enters the subarachnoid space.

The following procedure takes a midline approach. Non-midline approaches are covered in the reference text Wildsmith, Armitage and McClure (2002).
Stage 3
The needle’s obturator is removed and cerebrospinal fluid flows back and drips from the hub.
The following procedure takes a midline approach. Non-midline approaches are covered in the reference text Wildsmith, Armitage and McClure (2002).
Stage 4
A syringe of local anaesthetic solution is attached. On aspiration, a swirling pattern may be observed in the syringe because of the differing optical densities of the local anaesthetic solution and cerebrospinal fluid. The local anaesthetic is injected slowly and further aspiration may be performed to confirm continued correct placement. There should be no pain on injection. Drug doses are covered separately, but a typical solution would be 2-3 ml 0.5% hyperbaric bupivacaine, often with an added opioid. Needle and introducer are removed together.