Patient Factors
Patient factors which may lead to hypoxaemia are:
Respiratory drive
| Inadequate minute ventilation in spontaneously ventilating patients. | → |
This may be due to opioids, excessive depth of anaesthesia and residual muscle relaxation. |
| Most theatre ventilators do not currently allow synchronization of IPPV with patient breathing. | → |
Respiratory efforts by the patient during IPPV can impair ventilation. This can be avoided by ensuring adequate anaesthesia and muscle relaxation. |
Table 1 Respiratory drive can interfere with ventilation
Patient factors which may lead to hypoxaemia are:
Laryngospasm
Laryngospasm may be provoked by stimulation of the airway during light planes of anaesthesia by airway instrumentation, blood, secretions or volatile anaesthetic agents. Strong surgical stimuli away from the larynx, such as anal dilatation, may also produce laryngospasm if the depth of anaesthesia is inadequate.
Complete laryngospasm will be silent.
More usual is partial laryngospasm which is easily recognizable by the characteristic inspiratory sound. It usually responds to increasing the depth of anaesthesia, (e.g. boluses of IV propofol) or muscle relaxation (give suxamethonium if dangerous hypoxaemia is present or impending). Application of gentle CPAP with 100 % oxygen may improve oxygenation until the above takes effect.
Be aware that stomach inflation may occur as a result of attempted positive pressure ventilation against a closed glottis.
Patient factors which may lead to hypoxaemia are:
- Respiratory drive
- Laryngospasm
-
Lower airways obstruction:
- May result from bronchospasm or accumulation of secretions
- Is more likely in patients with hyper-reactive airways (smokers, asthmatics, recent LRTI)
- Bronchospasm can be provoked by drugs (e.g. atracurium, NSAIDs or beta blockers) or may be part of a systemic reaction, e.g. anaphylaxis
- Secretions should be removed by suction
- Bronchodilators may be given via either inhaled or parenteral routes
- Tension pneumothorax
- Alveolar gas exchange impairment

Patient factors which may lead to hypoxaemia are:
- Respiratory drive
- Laryngospasm
- Lower airways obstruction
- Tension pneumothorax
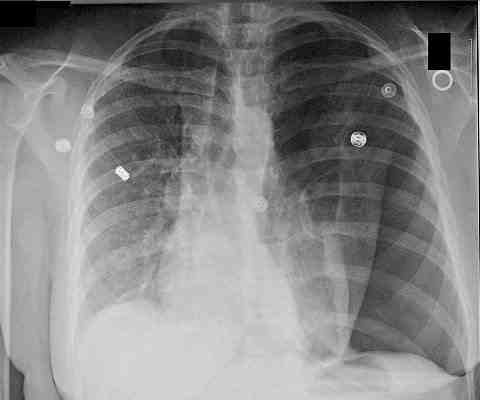
Tension pneumothorax may occur rarely during anaesthesia, presenting with hypoxia, difficulty with ventilation or hypotension.
Risk factors include chest trauma, bullous lung disease, subclavian CVC placement or brachial plexus block, as well as laparoscopic and thoracic surgery. - Alveolar gas exchange impairment
Patient factors which may lead to hypoxaemia are:
- Respiratory drive
- Laryngospasm
- Lower airways obstruction
- Tension pneumothorax
- Alveolar gas exchange impairment
Question: Hypoxaemia may occur in the face of apparently normal ventilation. What may cause this?
Click here for the answer.
Patient factors which may lead to hypoxaemia are:
- Respiratory drive
- Laryngospasm
- Lower airways obstruction
- Tension pneumothorax
- Alveolar gas exchange impairment
Question: Hypoxaemia may occur in the face of apparently normal ventilation. What may cause this?
Answer:
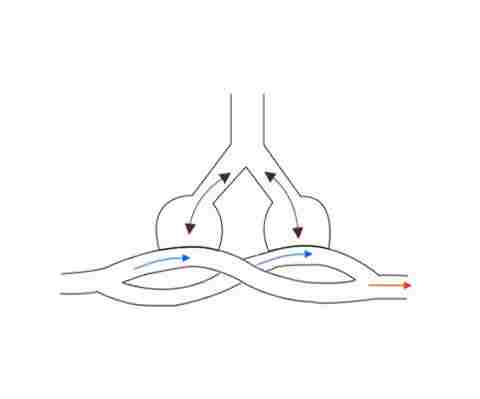
Ventilation/perfusion mismatch causing shunt. V/Q mismatch results when ventilation of areas of the lung is inadequate to fully oxygenate blood flow. Shunting occurs when blood passes though areas of the lungs that have no ventilation. Causes include, alveolar collapse and bronchial intubation.
Shunt will not be corrected by increasing the FiO2.
Patient factors which may lead to hypoxaemia are:
- Respiratory drive
- Laryngospasm
- Lower airways obstruction
- Tension pneumothorax
- Alveolar gas exchange impairment
Question: Hypoxaemia may occur in the face of apparently normal ventilation. What may cause this?
Answer:
Ventilation/perfusion mismatch causing shunt. V/Q mismatch results when ventilation of areas of the lung is inadequate to fully oxygenate blood flow. Shunting occurs when blood passes though areas of the lungs that have no ventilation. Causes include, alveolar collapse and bronchial intubation.
Shunt will not be corrected by increasing the FiO2.
Risk factors affecting V/Q mismatch
- Surgical factors:
- Pneumoperitoneum
- Surgical pressure on the chest
- Head-down tilt
- Patient factors:
- Lung disease
- Obesity
- Old age